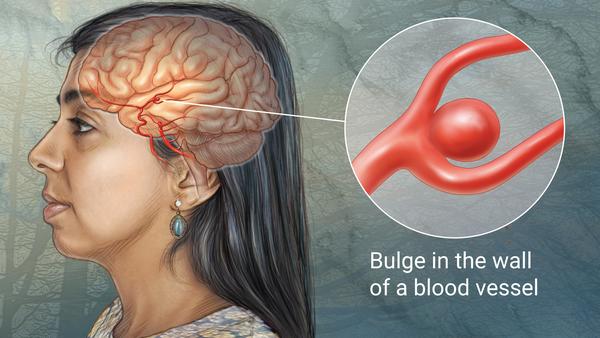
 Ever since their description in 1765, intracranial aneurysms have thrown a fascinating challenge at generations of neurosurgeons. The management of these lesions has been a saga of agony and ecstasy, trials and tribulations, achievements and tragedies. Often, the clipping of a difficult intracranial aneurysms elevates the neurosurgeon to the flight of Icarus, to be often followed by sobering self realization when faced with its sequelae like infarction, brain swelling, haemorrhage, etc. First pathological description of an intracranial aneurysm came from an autopsy of a patient who had died of apoplexy.(1) Modern era in the management of intracranial aneurysms dates from the publications of Sir Charles Symonds, which established subarachnoid haemorrhage as a distinct and important entity.(2) Introduction of cerebral angiography by Egas Moniz in 1927 made it possible to visualize the aneurysm preoperatively. Norman Dott carried out the first ever planned obliteration of the aneurysm by wrapping it with muscle in 1933. On March 23, 1937, Walter Dandy carried out a landmark surgery, when he clipped the neck of a posterior communicating artery aneurysm with a silver clip. Thereafter, aided by technical and technological advances, improvements in anaesthesia, introduction of clinical grading system, improvements in imaging and critical care and in perioperative brain protection techniques, postoperative mortality and morbidity after aneurysm surgery has shown a progressively downward trend.(3,4) Nevertheless, aneurysm surgery, especially that for posterior circulation aneurysms has remained a high risk venture and there are constant endeavours to make the occlusion safe for the patient. Endovascular treatment of aneurysms with Guglielmi detachable coils (GDC) introduced in 1991 was a major breakthrough in the continuing efforts to minimize the mortality and morbidity associated with surgery of aneurysms.
Ever since their description in 1765, intracranial aneurysms have thrown a fascinating challenge at generations of neurosurgeons. The management of these lesions has been a saga of agony and ecstasy, trials and tribulations, achievements and tragedies. Often, the clipping of a difficult intracranial aneurysms elevates the neurosurgeon to the flight of Icarus, to be often followed by sobering self realization when faced with its sequelae like infarction, brain swelling, haemorrhage, etc. First pathological description of an intracranial aneurysm came from an autopsy of a patient who had died of apoplexy.(1) Modern era in the management of intracranial aneurysms dates from the publications of Sir Charles Symonds, which established subarachnoid haemorrhage as a distinct and important entity.(2) Introduction of cerebral angiography by Egas Moniz in 1927 made it possible to visualize the aneurysm preoperatively. Norman Dott carried out the first ever planned obliteration of the aneurysm by wrapping it with muscle in 1933. On March 23, 1937, Walter Dandy carried out a landmark surgery, when he clipped the neck of a posterior communicating artery aneurysm with a silver clip. Thereafter, aided by technical and technological advances, improvements in anaesthesia, introduction of clinical grading system, improvements in imaging and critical care and in perioperative brain protection techniques, postoperative mortality and morbidity after aneurysm surgery has shown a progressively downward trend.(3,4) Nevertheless, aneurysm surgery, especially that for posterior circulation aneurysms has remained a high risk venture and there are constant endeavours to make the occlusion safe for the patient. Endovascular treatment of aneurysms with Guglielmi detachable coils (GDC) introduced in 1991 was a major breakthrough in the continuing efforts to minimize the mortality and morbidity associated with surgery of aneurysms.
To evaluate the comparative efficacy and safety of GDC coils with that of surgical clipping, International Subarachnoid Aneurysm Trial (ISAT) was designed and carried out in centers across several countries of Europe and North America.(5) This randomized multicentre trial compared neurosurgical clipping versus endovascular coiling in 2143 patients with aneurismal SAH. Clinical outcomes were assessed at two months and one year by assigning the modified Rankin scale (MRS) score. It was reported that 23.7% patients of the endovascular group were dependent or dead (MRS 3-6), compared to 30.1% patients of group with surgical clipping. Based on these results, the authors concluded that endovascular coiling offers better option in terms of survival and quality of life as compared to clipping in groups matched for other variables. The fact that the publication demonstrated superior results of non-surgical treatment has led to its intense scrutiny by neurosurgeons, literally setting cat among the pigeons. Close scrutiny of the ISAT revealed many unanswered issues and several flaws in the study that were glossed over. For instance, the basic design of the study was not adhered to, the samples were probably non-representative: majority of the aneurysms were good grade anterior circulation aneurysms. Moreover, of the 9559 patients with SAH assessed, 7416 (77.6%) were excluded, and only 2143 patients (22.4%) were randomized. On follow-up, there was a high rebleeding rate among the patients undergoing coiling, and the “safe and noninvasive” treatment is more likely to have the “dangerous” fatal consequence. Thus, the ISAT has been deemed to be a flawed study with a bias towards promotion of GDC coils.(6)
There have been other, major studies that have evaluated the efficacy of coils vis-à-vis surgical clipping. Murayama et al published their 11-year experience with GDC embolization of cerebral aneurysms.(7) In their series, 916 aneurysms were treated in 818 patients of which only 55% of the patients had complete occlusion at the time of treatment. In follow-up, overall recanalization rate was 20.9%, with a high of 59.1% in giant aneurysms. Overall morbidity and mortality for the series was 9.4%. In another study on 101 patients with unruptured intracranial aneurysms selected for coil embolization, complete aneurismal obliteration was achieved in 56% versus a 93.2% in surgical group.(8) Disregarding transient reversible postoperative complications, permanent complications were higher in the endovascular group at 7.5% versus 1.7% in the surgical group. Friedman et al retrospectively analyzed their results with GDC for endovascular occlusion of acutely ruptured saccular aneurysms over a 10-year-period.(9) At follow-up angiography over a mean period of 11.6 months, 30% had complete occlusion, 26% had dog-ear remnant, 5% had residual neck and 3% had residual filling aneurysm. Significantly, 34% of the patients required two or more endovascular procedures to secure their aneurysms and three patients required open surgical intervention. All these studies refute the statement that endovascular coiling is as effective as direct clip reconstruction in completely obliterating the aneurysm. Moreover, the incidence of ischaemic complications after coiling is high: Pelz et al reported 28% incidence of thromboembolic events.(10)
Aneurysms of the posterior circulation, involving the vertebrobasilar system and their branches have traditionally been a challenging field, because of anatomical inaccessibility, and the gross neurological morbidity associated with intraoperative rupture and consequent dissection and clip application. Hence it has been concluded that aneurysms of the posterior circulation are better coiled than clipped. Review of literature however reveals different conclusions. In a large study of 111 patients with ruptured vertebrobasilar aneurysms treated by GDC coiling, spread over 10 years by Groden et al, follow-up angiography was done at one year in 53 and at 18 months in 59 patients.(11) It was observed that complete obliteration of the aneurysms was not achieved in 23 (21%) aneurysms, while enlargement of the neck or reopening of the aneurysm was noticed in 12 of the 53 aneurysms at 12-month follow-up. Nine patients with angiography at 18 months or later had to be retreated with GDC coils, and three patients had subarachnoid hemorrhage necessitating repeat endovascular procedures. In another series of basilar trunk aneurysms treated by endovascular coiling by Uda et al, near complete occlusion occurred in 85.4% patients.(12) The results of these two series does not indicate any clear cut advantage of coiling over surgical clipping in posterior circulation aneurysms.
What should be the strategy for “poor risk” cases? In a comparison of operative versus endovascular treatment of anterior circulation aneurysms, Groden et al found similar outcomes in the two groups: out of 41 patients, 20 were treated by surgery and 20 by endovascular techniques and one patient received both the modalities of treatment.(13) Good outcomes were achieved in 6 of surgically treated and six of the coiled patients. However, the presence of haematoma was an indication for operative intervention, since the evacuation of the haematoma would not be possible by endovascular techniques. Clipping by microneurosurgical techniques remains the gold standard for assessment of aneurismal occlusion and rebleeding. The argument that endovascular techniques are less demanding and requirement of hospital resources is less is simply not true. The ICU stay is more a function of the neurological status than the intervention carried out. Add to this the requirement of frequent monitoring by angiography and the figures in terms of expenditure involved can be quite sobering. In a study on 171 patients (68 endovascular treatment and 103 surgical treatment), Niskanen et al compared the use of resources in the two groups. The median stay in ICU (1.7 v 1.8 days) and hospital stay (14 v 15 days) were similar.(14) The modality of treatment did not decrease the requirement of ICU beds or hospital stay. Clipping results in complete, permanent obliteration of the aneurysm, and does not have the obligatory requirement of regular angiographic follow-up. In India, often only one postoperative angiography is possible even in major, referral centers, and an annual study is generally not possible. Once the surgeon is past the learning curve, aneurysm surgery is done with high success rate and safety. The overall mortality rate of nearly 4.95% has been reported from a major center.(4) With the keyhole surgery getting refined, a number of these aneurysms can now be clipped with ease by keyhole, minimally invasive techniques aided by neuroendoscopy.
In summary, one can say that while surgical management of aneurysms has evolved and the microvascular techniques have become standardized, the endovascular techniques need to evolve further to be able to replace the established techniques of aneurysm obliteration. Coiling thus far has demonstrated a number of shortcomings when compared to microsurgical clip reconstruction. Direct clip application is associated with higher rate of permanent aneurysm obliteration. Endovascular techniques need not be looked as a panacea for management of aneurysms. In fact, surgery and endovascular techniques should be taken as complementary techniques, and the patients are best served with both the modalities available. The goal should not be to establish the superiority of one technique over the other, but both the techniques should be used synergistically and individually. Aneurysms have been operated for nearly 70 years, and surgery is firmly established as a definitive procedure for aneurismal obliteration. On the other hand, GDC coils were introduced only recently, and their long-term efficacy needs to be evaluated further. With the passage of time, we will see the march of technology translating into the aneurysms being treated with less and less of invasive techniques, whether surgical or endovascular. It is for the physicians to further refine and evolve the techniques that they are practicing and achieve low morbidity and improved clinical outcome.
REFERENCES
1. Bull J. A short history of intracranial aneurysms. Lond Clin Med J 1962; 3:47-51.
2. Symonds CP. Contributions to the clinical study of inracranial aneurysms. Guy Hosp Rep 1923; 73:129-32.
3. Yasargil MG. Microneurosurgery: Clinical considerations, surgery of intracranial aneurysms and results. Stuttgart: Georg Thieme; 1984.
4. Misra BK. Clipping versus coiling for the treatment of aneurysms: An overview. Ind J Cerebrovasc Surg 2005, 1:2-5.
5. ISAT collaborative group: International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysm: A randomized trial. Lancet 2002, 360:1267-74.
6. Barrow Daniel L. Bad science ISAT: The impact on Neurosurgery. Clin Neurosurg 2004; 51:126-31.
7. Murayama Y, Nien YL, Duckwiler G, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11-years’ experience. J Neurosurg 2003, 98:959-66.
8. Raftapoulos C, Goffette P, Vaz G, et al. Surgical clipping may lead to better results than coil embolization. Results from a series of 101 consecutive unruptured intracranial aneurysms. Neurosurgery 2003, 52:1280-7.
9. Friedman JA, Nichols DA, Meyer FB, et al. Guglielmi detachable coil treatment of ruptured saccular cerebral aneurysms: Retrospective review of a 10-year single center experience. AJNR 2003, 24:526-33.
10. Pelz DM, Lownie SP, Fox AJ. Thromboembolic events associated with the treatment of cerebral aneurysms with Guglielmi detachable coils. AJNR 1998, 19:1541-7.
11. Groden C, Eckert B, Ries T, Probst TN, Kucinski T, Zeumer H. Angiographic follow-up of vertebrobasilar aneurysms treated with detachable coils. Neuroradiology 2003, 45:435-440.
12. Uda K, Murayama Y, Gobin YP, Duckwiler GR, Vinuela F. Endovascular treatment of basilar artery trunk aneurysms with Guglielmi detachable coils: Clinical experience with 41 aneurysms in 39 patients. J Neurosurg 2001, 95:624-632.
13. Groden C, Kremer C, Regelsberger J, Hansen HC, Zeumer H. Comparison of operative and endovascular treatment of anterior circulation aneurysms in patients in poor grades. Neuroradiology 2001, 43:778-783.
14. Niskanen M, Koivisto T, Ronkainen A, et al. Resource use after subarachnoid haemorrhage: Comparison between endovascular and surgical treatment. Neurosurgery 2004, 54:1081-6.

Leave a Reply